When your hands swell up in the morning, your knees ache for no clear reason, and your joints feel stiff even after resting, it’s not just aging - it could be lupus arthritis. This isn’t ordinary arthritis. It’s a symptom of systemic lupus erythematosus (SLE), an autoimmune disease where your immune system attacks your own tissues. About 90% of people with lupus will experience joint pain and swelling at some point. And for most, the go-to treatment isn’t a powerful steroid or a costly biologic - it’s a small, inexpensive pill called hydroxychloroquine, sold under the brand name Plaquenil.
What Makes Lupus Arthritis Different?
Lupus arthritis doesn’t destroy bone like rheumatoid arthritis does. Instead, it causes inflammation in the lining of the joints - the synovium - leading to pain, swelling, and stiffness, mostly in the small joints of the hands, wrists, and knees. The inflammation is often symmetric, meaning if your left wrist hurts, your right one will too. Morning stiffness can last for hours, and flare-ups come and go without warning. But unlike other forms of arthritis, lupus arthritis rarely leads to permanent joint damage. That’s one reason why doctors don’t rush to use harsh drugs right away.
The real danger isn’t just the joint pain - it’s what’s happening inside your body. Lupus triggers your immune system to overreact. It produces autoantibodies, releases inflammatory chemicals like TNF-alpha and interleukin-6, and activates immune cells in ways that harm organs over time. That’s why treating lupus arthritis isn’t just about relieving pain - it’s about stopping the disease from spreading to your kidneys, heart, or brain.
Why Hydroxychloroquine Is the First-Line Treatment
Hydroxychloroquine has been around since the 1940s, originally developed as an antimalarial drug. But in the 1950s, doctors noticed that patients with lupus and rheumatoid arthritis who took it for malaria had fewer flare-ups. That accidental discovery changed everything. Today, according to the American College of Rheumatology, 85-90% of people with lupus are prescribed hydroxychloroquine. The European League Against Rheumatism gives it the highest recommendation grade - A - meaning the evidence is rock solid.
It’s not a miracle cure. It doesn’t work overnight. But over time, it does something few other drugs can: it reduces inflammation, prevents flares, and protects your organs - all with fewer side effects than steroids or immunosuppressants.
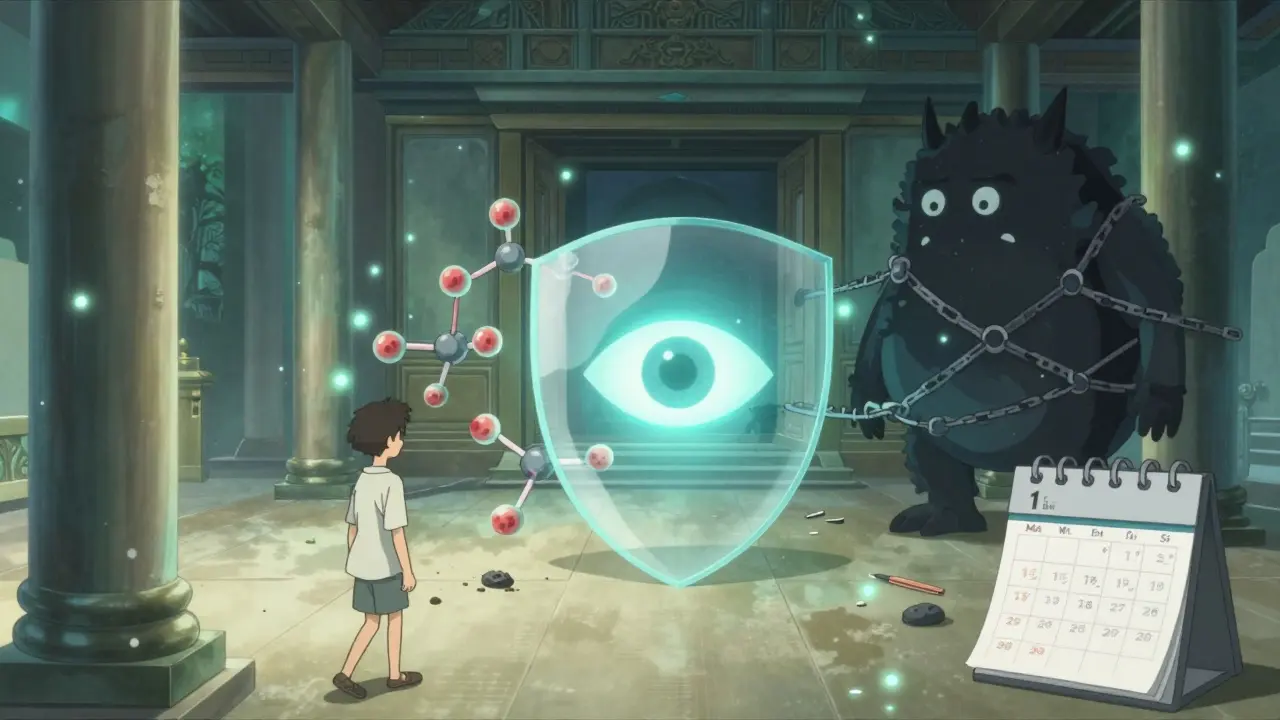
How Hydroxychloroquine Actually Works
Hydroxychloroquine doesn’t just numb pain. It changes how your immune system behaves at a cellular level. Inside your immune cells, it raises the pH in compartments called endosomes. This disrupts key signals that tell your body to attack itself. Specifically, it blocks Toll-like receptors (TLR7 and TLR9), which are like alarm bells that go off when your immune system detects what it thinks is a virus - even when there isn’t one.
By quieting these alarms, hydroxychloroquine reduces the production of interferons and other inflammatory proteins by 35-40%. It also cuts down on TNF-alpha and interleukin-6 by 20-30%. These are the exact chemicals that cause joint swelling and fatigue. In lab studies, it even reduces oxidative stress by 30-35%, which helps protect blood vessels and lowers your risk of heart disease - a major concern for lupus patients.
Another underrated benefit? It helps regulate autophagy - the process where cells clean up damaged parts. In lupus, this process goes haywire, and hydroxychloroquine brings it back into balance. That’s why it’s not just treating symptoms - it’s slowing the disease itself.
Real Results: What Patients Experience
On forums like the Lupus Foundation of America’s community, 68% of users report moderate to significant improvement in joint pain after 3-6 months on hydroxychloroquine. One user, LupusWarrior87, wrote: “After 4 months on 300mg Plaquenil, I went from needing 10mg prednisone daily to zero steroids with dramatically less morning stiffness.”
That’s not rare. In clinical studies, 62% of patients show measurable improvement in joint counts by 12 weeks. By six months, that number jumps to 85%. Many people stop needing daily steroids. Others notice fewer hospital visits and less fatigue.
But it takes patience. Unlike prednisone, which can reduce swelling in days, hydroxychloroquine needs 8-12 weeks to start working. Some patients give up too soon. One study found that 25% of people stop taking it in the first year because they don’t see immediate results. That’s a mistake. The benefits build slowly - and they last.
How It Compares to Other Treatments
Let’s say your joints are really inflamed. Your doctor might consider methotrexate, a traditional arthritis drug. Methotrexate can be slightly more effective at reducing active synovitis - but it’s harder on your liver. You need monthly blood tests. And it can cause nausea, fatigue, and even lung issues in rare cases.
Biologics like belimumab work well for severe lupus, but they cost $45,000 a year. Hydroxychloroquine? $600-$1,200 a year, even with the brand name. Generic versions cost as little as $0.45 per pill. And unlike biologics, which suppress your immune system broadly, hydroxychloroquine is more selective. It doesn’t leave you vulnerable to every infection.
Corticosteroids? They work fast - but they’re a double-edged sword. Long-term use increases your risk of osteoporosis by 40%. Hydroxychloroquine does the opposite: it actually improves bone density by 3-5% over two years. That’s huge for people with lupus, who are already at higher risk for bone loss.
Protecting More Than Just Your Joints
The real power of hydroxychloroquine isn’t just in the joints. It protects your whole body.
People with lupus often have antiphospholipid syndrome - a condition that makes blood clot more easily. Hydroxychloroquine reduces clotting events by 30-35%. That means fewer strokes, fewer pulmonary embolisms, fewer miscarriages.
It also improves cholesterol. Studies show it lowers total cholesterol by 10-15 mg/dL and raises “good” HDL cholesterol by 5-10 mg/dL. That’s equivalent to the effect of a low-dose statin - without the muscle pain or liver concerns.
And here’s something most people don’t know: hydroxychloroquine cuts your risk of serious infections by 95% compared to those not taking it. That’s because it doesn’t wipe out your immune system. It just calms down the parts that are misfiring.
The Big Concern: Eye Safety
No drug is perfect. The biggest worry with hydroxychloroquine is retinal toxicity - damage to the retina that can lead to vision loss. But here’s the truth: it’s rare, and it’s preventable.
The risk is less than 1% in the first five years of use. After five years, it rises slightly - to about 7.5% in people taking more than 5 mg per kilogram of body weight daily. That’s why dosing matters. The standard is 5 mg per kg of real body weight, capped at 400 mg per day. For a 70 kg person, that’s 350 mg max. Many doctors start at 200 mg and increase slowly.
Screening is key. The American Academy of Ophthalmology recommends a baseline eye exam within the first year of starting hydroxychloroquine. After five years, you need annual exams. If you have kidney disease, are on tamoxifen, or have a family history of eye problems, you might need screening sooner.
Thanks to new tools like the AdaptDx Pro dark adaptometer, doctors can now detect early changes in retinal function before vision loss happens. False negatives have dropped by 35%. So if you’re getting screened properly, your risk of permanent damage is extremely low.
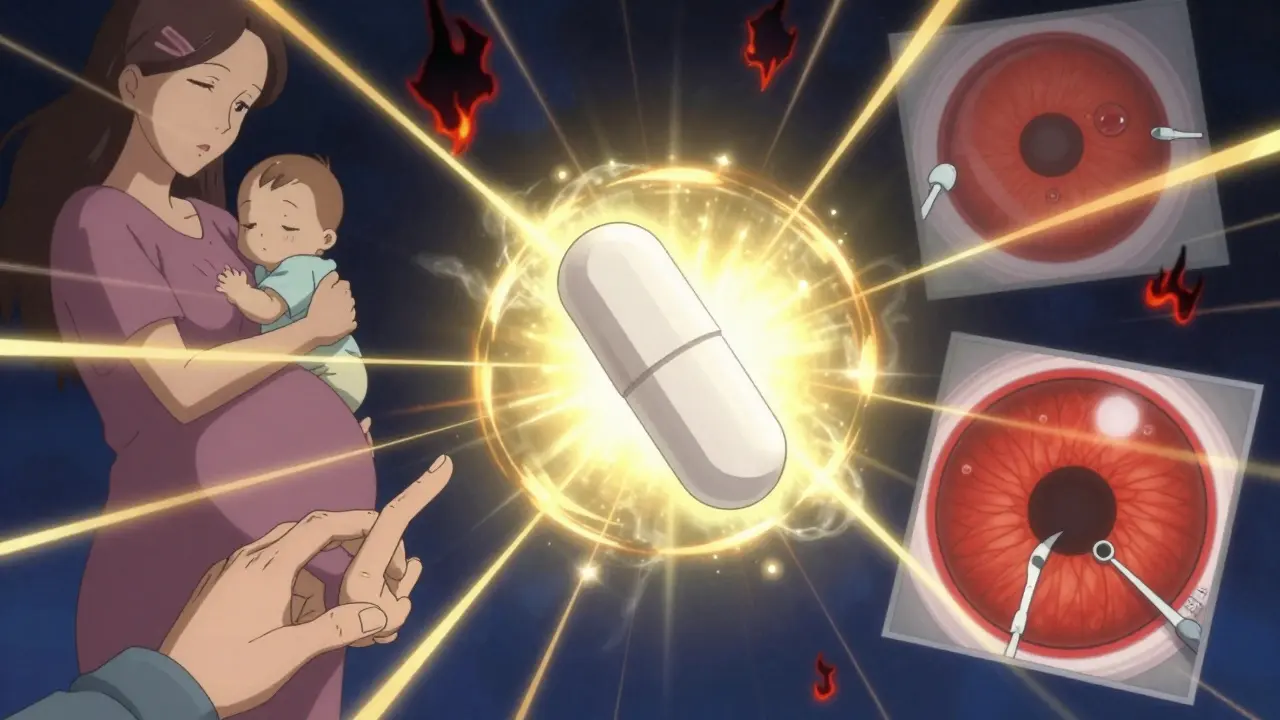
What About Pregnancy and Kids?
Hydroxychloroquine is one of the safest drugs for pregnant women with lupus. In the PROMISSE study, women who stayed on hydroxychloroquine during pregnancy had fewer flares, fewer preterm births, and healthier babies. About 78% of pregnant lupus patients are prescribed it - compared to only 65% of non-pregnant adults.
For children with lupus, it’s even more common. Ninety-four percent of pediatric lupus patients take hydroxychloroquine. Why? Because it doesn’t stunt growth, doesn’t weaken bones like steroids do, and doesn’t increase infection risk like stronger immunosuppressants. It’s the go-to for long-term control.
Practical Tips for Taking Hydroxychloroquine
- Dose wisely: Stick to 5 mg per kg of body weight per day. Don’t exceed 400 mg daily. For most people, 200-300 mg daily is enough.
- Be patient: Give it at least 3-6 months. Don’t quit if you don’t feel better in 6 weeks.
- Get your eyes checked: Baseline exam within a year. Annual exams after five years. Keep a record.
- Don’t switch generics randomly: A 2022 JAMA study found some generic versions have lower blood levels. If you’re stable on one brand, stick with it.
- Watch for side effects: Nausea, vivid dreams, or dizziness are common early on. They usually fade. Report blurred vision, light sensitivity, or blind spots immediately.
- Use support tools: The Lupus Foundation of America’s “Plaquenil Passport” app helps track doses and appointments. The American College of Rheumatology’s “Understanding Your Lupus Medications” module is free and excellent.
The Future of Hydroxychloroquine in Lupus
Even after 70 years, hydroxychloroquine keeps surprising researchers. New studies show it may influence epigenetics - turning off genes that drive inflammation. It might also change your gut microbiome in ways that reduce autoimmune activity.
Right now, clinical trials are testing it in combination with newer drugs like anifrolumab. Early results show a 45% greater reduction in disease activity compared to hydroxychloroquine alone. That could mean even better outcomes for people with moderate to severe lupus.
Meanwhile, scientists are developing biomarkers to predict who will respond best. If your interferon gene signature normalizes after three months on hydroxychloroquine, you’re likely to do well long-term. That’s the future: personalized treatment based on your biology, not guesswork.
For now, hydroxychloroquine remains the most important drug in lupus care. It’s not flashy. It doesn’t make headlines. But for millions of people, it’s the reason they can still hold their grandchild’s hand, type on a keyboard, or walk without pain. It’s not a cure - but it’s the closest thing we have to a shield against the storm of lupus.
How long does it take for hydroxychloroquine to work for lupus arthritis?
Most people start noticing less joint pain and stiffness after 8-12 weeks, but full benefits usually take 3-6 months. This delay is normal - hydroxychloroquine works by changing how your immune system behaves over time, not by masking pain like a painkiller. Stopping too early because you don’t see quick results is the most common reason people don’t benefit.
Can I stop taking hydroxychloroquine if my symptoms improve?
No. Even if your joints feel fine, stopping hydroxychloroquine increases your risk of a severe lupus flare by 50-70%. It’s a maintenance drug - not a rescue one. Doctors recommend staying on it indefinitely unless you have a serious side effect. Many patients take it for decades without issues.
Is hydroxychloroquine safe for long-term use?
Yes, for most people. Studies tracking patients for over 20 years show that with proper dosing and regular eye exams, long-term use is safe and effective. The biggest risk is retinal toxicity, but that’s rare - under 1% in the first 5 years and under 2% after 10 years when dosing guidelines are followed. The benefits - reduced flares, lower infection risk, heart protection - far outweigh the risks for the vast majority.
Why do some people say hydroxychloroquine doesn’t work for them?
Some people don’t respond because their lupus is driven by different immune pathways. Others stop too soon or take inconsistent doses. A small group may have genetic variations that affect how their body processes the drug. If you’ve been on it for 6 months with no improvement, talk to your rheumatologist. They may add another medication - but rarely will they stop hydroxychloroquine entirely, since it’s still protecting your organs.
Are generic versions of hydroxychloroquine as good as Plaquenil?
Most generics are fine, but a 2022 study in JAMA Internal Medicine found that some generic brands result in 18% lower blood levels of the drug. That could mean less effectiveness. If you switch generics and notice your symptoms returning, talk to your doctor. Many rheumatologists recommend sticking with the same manufacturer - whether brand or generic - to ensure consistent dosing.
Does hydroxychloroquine help with lupus fatigue?
Yes. While it’s not a stimulant, many patients report reduced fatigue after 3-4 months on hydroxychloroquine. This isn’t just from less joint pain - it’s because the drug lowers overall immune system activation. When your body isn’t constantly fighting itself, you have more energy. In one study, 68% of users reported feeling less tired after six months.
Can hydroxychloroquine prevent lupus from developing?
There’s some evidence it might. In people with positive lupus antibodies but no symptoms, hydroxychloroquine reduced the chance of developing full-blown lupus by 58% in one study. But a larger 2022 trial (ASAS PREVENT) found no significant difference over 24 months. The jury is still out. Right now, it’s not approved for prevention - only for treating diagnosed lupus.
What should I do if I miss a dose of hydroxychloroquine?
If you miss a dose, take it as soon as you remember - unless it’s close to your next scheduled dose. Don’t double up. Missing one dose won’t undo your progress, but frequent missed doses can make the drug less effective and increase flare risk. Set phone reminders or use a pill organizer. Consistency matters more than perfection.
What’s Next?
If you’re on hydroxychloroquine, keep taking it. Keep your eye appointments. Talk to your doctor if you notice new symptoms - especially vision changes, heart palpitations, or muscle weakness. If you’re not on it yet and have lupus arthritis, ask your rheumatologist why not. It’s the most studied, safest, and most protective drug in your treatment plan. It’s not the loudest, but it’s the one that’s been saving lives for decades.

Aadil Munshi
December 18, 2025 AT 23:47